Envita’s Proprietary PathoDNA Test for The Diagnose Lyme Disease and
Co-Infections
Lyme disease remains an epidemic in the United States. It is the most commonly reported vector-borne disease in
America
with as many as 300,000 people per year being affected according to the most recent surveillance data released by the
CDC [1]. As temperatures rise, the areas where the disease is prevalent are likely to grow due to new regions becoming
hospitable for vectors such as the long-horned tick [2]. This means more and more people are being exposed to Lyme
disease each year. Despite the growing public threat, our officially recognized means of diagnosing Lyme disease
remains
poor in its efficiency.
Recognizing the poor sensitivity of Western blot and ELISA in detecting the early stages of Lyme disease, the CDC
currently mandates a two-tiered approach utilizing both methods in an attempt to improve sensitivity. Despite this,
sensitivity remains as low as 29-40% for early Lyme disease [3]. Ordinarily, a sensitivity of 95-99% is required for a
confirmatory test, yet many doctors are not aware of the poor performance of the CDC-mandated test for Lyme.
A combination of factors such as immune evasion, biofilms, and low population result in the high difficulty of
confirming the presence of the bacteria that causes Lyme disease, Borrelia Burgdorferi. As well, the two-tiered test
is
not looking for the organism directly, but rather for antibodies produced in response to borreliosis. It is no
surprise
that immune complications caused by Borrelia result in weak or muddled signals when searching for the complementary
human antibodies. What we need is a new approach to detection, one that involves direct detection of the Lyme bacteria
itself.
Enter PathoDNA, a next-generation DNA sequencing test designed specifically for the detection of Lyme disease and its
associated coinfections, released by Genetic First Laboratories in association with Unipathic Medicine and Envita
Medical Centers. Next-generation sequencing is a more advanced technology than Western blot and ELISA and is
potentially
millions of times more sensitive than the older tests.
By analyzing the DNA contained in a sample down to each base pair, this new diagnostic test directly detects Borrelia
Burgdorferi and the most common tick-borne infections by comparing their sequences to a patented DNA library.
The test is hypothesis-free, meaning that the doctor no longer has to guess at which infection(s) their patient has
before ordering a test. PathoDNA will print out a quantified list of detected organisms from the sample.
Now is the time for Lyme disease to move out of the shadows with the light of new, advanced technology. It’s time to
recognize the threat Lyme poses to the public health and to counteract it with means that are efficient and effective.
PathoDNA, Next Level Tick-Borne Infectious Screening
PathoDNA by GeneticFirst is a CLIA validated NGS (next-generation sequence test) for the diagnosis of Lyme disease
(Borrelia Burgdorferi) and other secondary tick-borne co-infections. PathoDNA involves a robust patent-pending
bioinformatic process that tests for pathogens at a higher accuracy than using traditional testing methods. This
greater
accuracy is accomplished by testing for the actual genetic information of the organisms of highest concern as opposed
to
the typical antibody (immune system) based tests, such as western blot, which are less than 20% accurate in the acute
phase of disease and 70% accurate in the chronic phase of disease.
The test was created in partnership with Envita Medical Centers via research and development with thousands of
samples
tested to provide the most accurate testing and symptomatic tracking using the PathoDNA testing method.
Understanding Next-Generation Sequencing
Another term for Next-Generation Sequencing (NGS) is “massively-parallel sequencing.” The name means that rather than
sequencing a single strand of DNA or RNA from start to finish, many strands are sequenced simultaneously. Breaking a
single long strand of DNA into multiple small pieces that can all be processed at the same time is a way to get
through
the task of sequencing quickly.
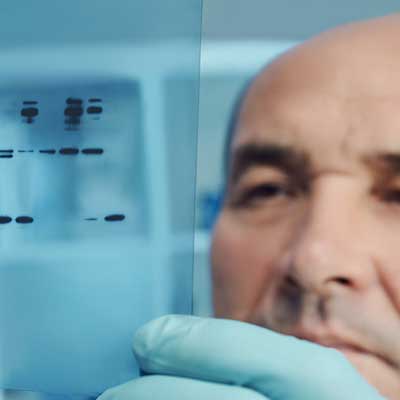
Traditional sequencing, or “Sanger sequencing” by capillary electrophoresis is still used for small sets of gene
targets
and is often considered the “gold standard” in DNA sequencing. Sanger sequencing is also sometimes used to verify the
results of NGS.
NGS technology combines high accuracy with high throughput, increasing the speed of genetic sequencing analyses. NGS
enables hundreds to thousands of genes to be interrogated at once across multiple samples. Discovery and analysis of
different genomic features can take place in a single sequencing run, something which is simply not possible with
older
techniques.
Research utilizing NGS can more easily find genetic features such as single nucleotide variants (SNVs), copy numbers,
structural variations, and RNA fusion events. By processing many strands at once, the speed at which studies can be
completed greatly increased. Additionally, NGS has lower sample input requirements than older techniques and the
ability
to detect variations at lower allele frequencies than is possible with Sanger sequencing.
NGS is a powerful tool with a variety of applications. At Envita Medical Centers, NGS is key to our strategy for
detecting infectious microorganisms, especially hard-to-detect pathogens like Borrelia Burgdorferi, the organism the
causes Lyme Disease. For the purposes of clinical detection, it is important to find an NGS technology which is
specifically designed to the task and is CLIA validated. A higher-than-normal level of accuracy is needed for clinical
detection since B. Burgdorferi occurs at low populations in serum, and there may be too much noise in traditional
multiplex sequencing methods to make a sound diagnosis. Metagenomic sequencing technology allows for the necessary
level
of accuracy without the need for sequence specific amplification, which can miss some bacteria DNA fragments due to
low
population quantities.
For infectious diseases, NGS represents a major step forward in making the diagnosis. The technology allows for
doctors
to essentially “scan” for foreign DNA without the need to make a hypothesis or best guess first, dramatically speeding
up the diagnostic process. NGS has been used to confirm diagnoses in patients with unidentified infections, even after
negative results from conventional tests. Envita Medical Centers believes that NGS holds great promise for improving
disease diagnostics, especially for critically ill people and those with compromised immune systems. PathoDNA goes a
step farther than NGS alone by creating custom targets for identification.
PathoDNA is CLIA Validated Test
When a laboratory develops a test system such as an LDT in-house without receiving FDA clearance or approval, CLIA
prohibits the release of any test results prior to the laboratory establishing certain performance characteristics
relating to analytical validity for the use of that test system in the laboratory’s own environment. This analytical
validation is limited, however, to the specific conditions, staff, equipment, and patient population of the particular
laboratory, so the findings of these laboratory-specific analytical validations are not meaningful outside of the
laboratory that did the analysis. Furthermore, the laboratory’s analytical validation of LDTs is reviewed during its
routine biennial survey – after the laboratory has already started testing.
In contrast, the FDA’s review of analytical validity is done prior to the marketing of the test system, and
therefore,
prior to the use of the test system on patient specimens in the clinical diagnosis/treatment context. Moreover, the
FDA’s premarket clearance and approval processes assess the analytical validity of a test system in greater depth and
scope.
The FDA’s processes also assess clinical validity, which is the accuracy with which the test identifies, measures, or
predicts the presence or absence of a clinical condition or predisposition in a patient, as part of the review that is
focused on the safety and effectiveness of the test system. Furthermore, unlike the FDA regulatory scheme, CMS’ CLIA
program does not address the clinical validity of any test but repeatability. Thus, the two agencies’ regulatory
schemes
are different in focus, scope, and purpose, but they are intended to be complementary. It is important to note that
most
laboratory test are not FDA approved but CLIA validated.
Why CLIA Validation Matters
Most testing is not FDA approved but CLIA validated and in fact most test used to diagnosis Lyme disease using NGS
next
generation sequencing are not CLIA validated. Healthcare professionals are legally required to use CLIA validated test
prior to making medical diagnosis and treatment recommendations. Especially in the highly conversional Chronic Lyme
Disease space it is highly recommended to use the highest level of standards to protect patients.
Choose Envita Medical Centers
Call Now
Our team is ready to help you get your life back! Please enter your contact information and a
Patient Care Expert will
contact you shortly. If you would rather speak now, please give us a call at 866-830-4576.
References
[1] Schwartz, A. M., Hinckley, A. F., Mead, P. S., Hook, S. A., & Kugeler, K. J. (2017). Surveillance for Lyme
Disease —
United States, 2008–2015. MMWR Surveillance Summaries, 66(22), 1-12. doi:10.15585/mmw.ss6622a1
[2] Deresinski, S. (2019). The Longhorned Tick: Is It Coming to a Place Near You? Infectious Disease Alert,
38(4).
[3] Aguero-Rosenfeld, M. E., Wang, G., Schwartz, I., & Wormser, G. P. (2005). Diagnosis of Lyme Borreliosis.
Clinical
Microbiology Reviews, 18(3), 484. doi:10.1128/CMR.18.3.484-509.2005